Lived experience fuels compassionate recovery care
Credit: Giles Clasen
Story and photos by Giles Clasen
Sally Gibbens remembers her most frightening overdose. She had been using heroin and other drugs for years and overdosed a handful of times. Unmoved by those experiences, she refused to change the trajectory of her life.
But that changed in 2015. Gibbens had just picked up her friend Natalie and parked in a bowling alley parking lot in downtown Duluth, Minnesota.
Gibbens felt sick. It had been nearly a day and a half since she last scored her drug of choice. Now she was in the earliest phases of heroin withdrawal.
Natalie shot up first. Her eyes rolled to the back of her head, and she slumped moments after pushing the drug into her vein. Then, her breathing slowed. Gibbens recognized immediately that Natalie had overdosed, and her friend’s only chance of surviving was to get to a hospital as quickly as possible.
But she delayed making the trip to the hospital. She needed to get high first.
According to Gibbens, she thought to herself, “I’m too sick to drive. I’m going to do less than what Natalie did.” Gibbens needed the hit. Then, she would be able to drive Natalie to the ER.
“At the time, it was more important to me to get that fix than to take my friend to the emergency room,” Gibbens said.
Gibbens found a vein and coerced the needle in. She pushed the plunger. Once Gibbens felt the comfort of her high, she drove off, blood dripping down her arm. She turned right from the parking lot down a steep hill. Everything went dark within seconds.
Gibbens woke up in an ambulance screaming a wretched, desperate wail. She could see her car smashed into the Duluth library and paramedics trying to revive Natalie.
“I just knew there were going to be a lot of repercussions for my actions,” Gibbens said.
Discovering Urban Peaks
Today, Gibbens works as the office administrator for Urban Peaks Rehab. The small medical office, near Colfax and Park Avenues, specializes in offering medication-assisted treatment, or MAT, for opioid use disorder.
What sets Urban Peaks Rehab apart from other addiction treatment programs is that most of the small staff have faced opiate or opioid addiction. They understand what it is like to crave the drugs. They also know what it means to go through withdrawal and what life after drug use can look like.
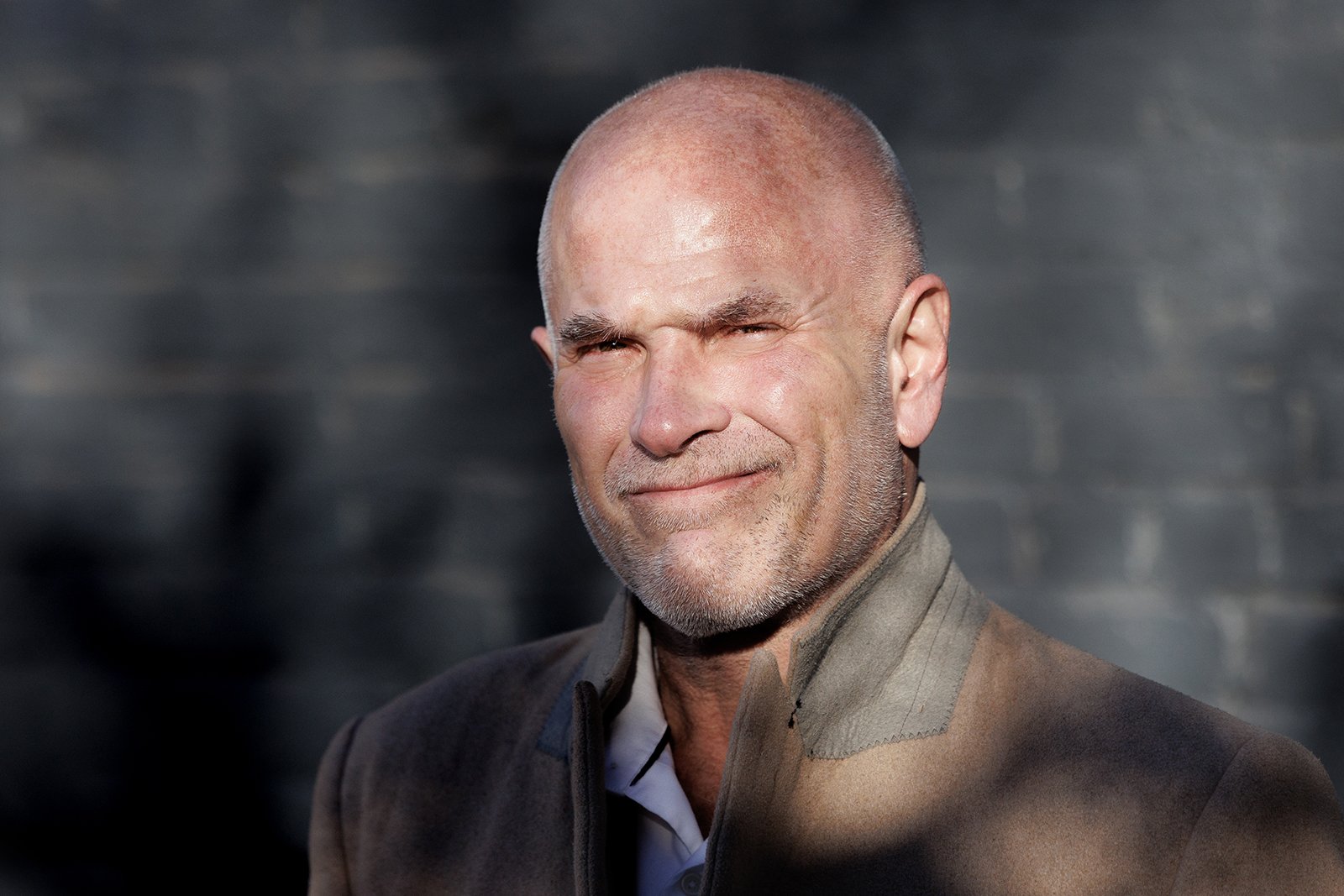
Urban Peaks Rehab’s founder and medical director, Dr. Chad Johnston, shifted his practice to addiction treatment after his own fight with opioids and opiates. He started using tramadol while working in the intensive care unit, just before his medical residency.
“I was working in the ICU, and we had this guy collect the meds and usually dispose of them,” Johnston said. “There was often some stuff left in there, and I started stealing the leftover pills.”
Johnston didn’t realize it at the time, but he was depressed. Throughout life, his father pushed him to succeed. The pressure made everything in Johnston’s life black and white, win or lose. Everything was a competition. Johnston had made most of his decisions to win his father’s affection.
In 1999, determined to please his father, Johnston upended his life to start medical school. He was 30 years old and one of the oldest in his class.
It took him years to acknowledge that his behavior was a problem.
“It was about two years or three years ago that I realized,” Johnston said. “The depression was out of control because nothing I did was enough. That pressure builds until you find a release. For me, sadly, my release was tramadol first, and later, morphine.”
When Johnston first took the tramadol, he thought it was a risk-free high. It was marketed as a synthetic opioid that worked differently on the brain than traditional prescription pain medications. This led researchers and the Food and Drug Administration to deem it a safe alternative to stronger painkillers like Percocet or Oxycontin.
With time, it became clear that tramadol came with its own baggage, and it proved to be addictive and destructive, too. In 2014, the Drug Enforcement Administration labeled tramadol a Schedule IV controlled substance.
“I can’t believe I didn’t know more about opiates,” Johnston said. “We had no training in medical school at all. I thought [tramadol] was safe, or at least safer.”
Johnston abused tramadol throughout his residency in 2003. He would prescribe too many pills for patients and pocket the extra. In a pinch, he ordered them online. When Johnston began his fellowship in hospice care, he moved from tramadol to liquid morphine. It was easy to steal the bottles from patients’ rooms, often after they died.
“I really enjoyed helping people at the end of their life, but it got me all sideways, all those drugs around,” Johnston said. “I was so selfish then. That’s what the drugs do. They make you so fucking selfish. It’s a selfishness that you can’t even describe.”
In 2010, Johnston decided he needed to get sober.
“That’s when my wife at the time came to me and said, ‘You know, we’re in a small town. Here’s the newspaper. Look at the front page. You’re going to be right there, and it’s going to say you’re a drug addict,’” Johnston said.
Johnston checked himself into a Florida rehab facility the following week. He doesn’t remember the exact cost of the facility but thought he spent in the neighborhood of $50,000- $80,000. Johnston said he knows he was lucky to be able to pay such high costs when so many others can’t.
“[My wife] knew I was that vain and that shallow,” Johnston said. “She knew what card to play to motivate me, and I applaud her for it. It was such a wonderful move because it saved my life, even if she did leave me later. Rightly so, probably.”
Creating a Patient-First Model
In rehab, Johnston began taking Suboxone to prevent drug cravings and avoid withdrawal symptoms. Suboxone was one of the first new MATs for opiate and opioid addiction. It is a daily treatment that can be prescribed by a doctor and taken at home.
It differs from methadone, another MAT, because of its ease of use. One must generally go to a methadone treatment center daily to receive their dose. This inconvenience with methadone treatment can lead to failure and relapse, while Suboxone can be taken safely outside of medical supervision.
For Johnston, Suboxone was a game changer. It helped him become and stay sober. But addiction had torn his life apart. He didn’t work for a year, and then, he tried returning to hospice care. It didn’t work for him.
Then, the clinic treating his addiction offered him a job. He changed the focus of his life to serving individuals who battled addiction like him.
Lured by Colorado’s beauty, Johnston moved to Denver. He founded Urban Peaks Rehab in 2018, with a vision to create a new patient-first model for addiction treatment.
Johnston appreciated what rehab had done for him, but after working in an addiction treatment clinic, he also saw how rehab was big business. According to Johnston, higher revenues in the industry were too heavily motivated by dollars rather than care.
Johnston realized that for many individuals, it was difficult to receive life-saving MAT treatment because of the costs and stigma. He heard stories about doctors putting up burdens to receive treatment. Many told Johnston that when they sought help, several medical professionals shamed them. Johnston even heard stories about patients being refused treatment because some doctors believed that if an individual got themselves into drug addiction, they had to pull themselves up by their bootstraps to get out of addiction.
“It makes no sense to me that providers would shame anyone who ever came into their office, but it happens all the time,” Johnston said. “We have these amazing treatments that make recovery easier and less painful than in the past and individuals struggle to find someone to prescribe [MATs] because of [the common conceptions] of who an addict is and what they deserve — which is nothing.”
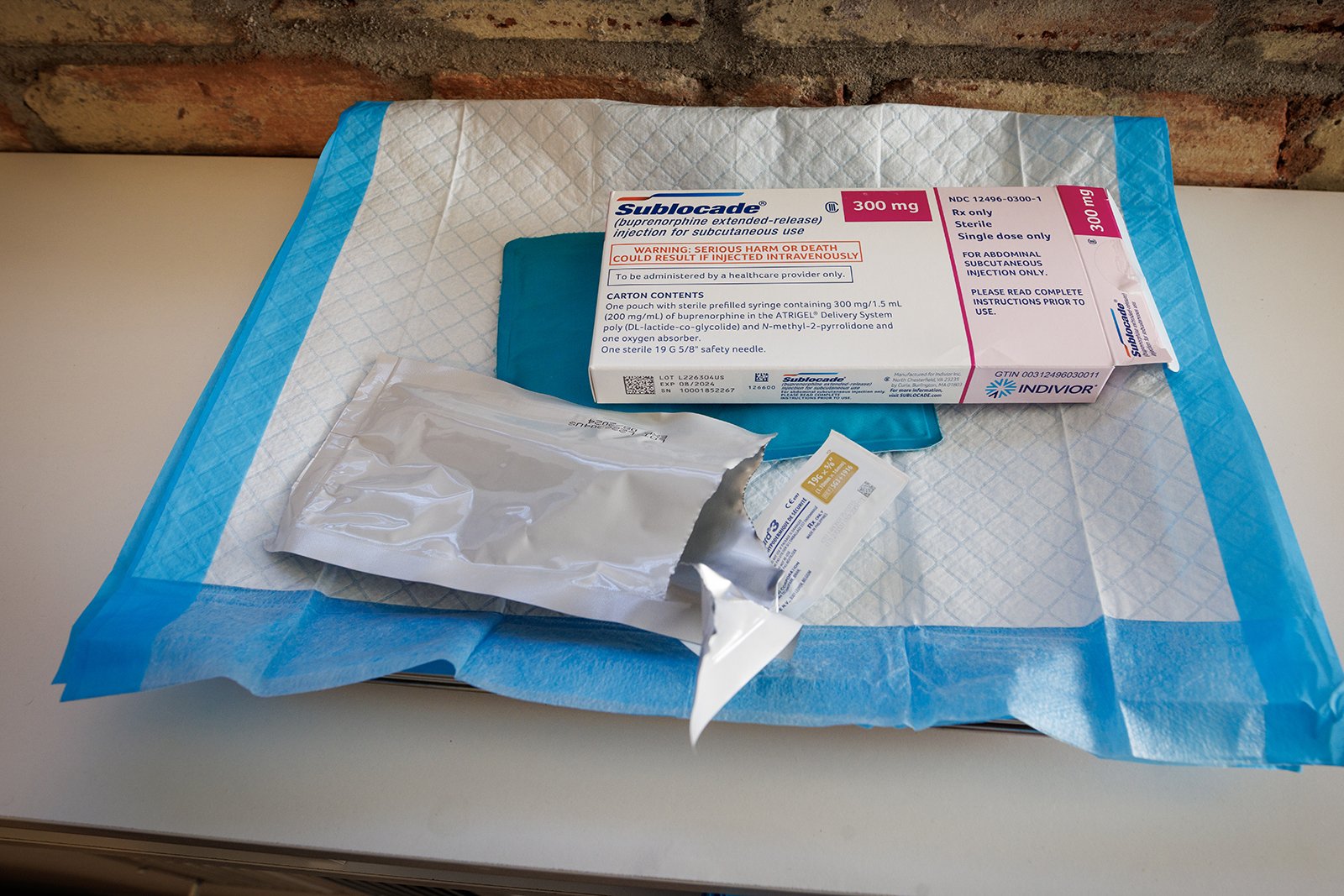
Johnston started a six-month treatment of Sublocade in 2023. Sublocade is a next-generation MAT treatment. Approved by the FDA in 2017, Sublocade is a monthly shot in the abdomen that slowly releases buprenorphine, the same active ingredient in Suboxone.
Johnston noted that the biggest difference between Sublocade and Suboxone is that Suboxone is a daily treatment taken in perpetuity. But with Sublocade, many can end treatment after six months without experiencing further cravings.
Medicaid and many insurance plans cover both treatments in Colorado, and the manufacturer has copay assistance programs. Outpatient MAT is an affordable treatment option compared to lengthy in-treatment programs. Johnston knows that most can’t afford the type of rehab he utilized because of the cost. He wants everyone to know that the treatment is available to almost anyone seeking recovery.
Johnston also believes MAT isn’t enough to help someone truly overcome their addiction. He has brought a counselor onto his team to help offer more extensive support and services to his patients. He and Gibbens want Urban Peaks Rehab to provide patients with a greater chance at overcoming addiction.
The clinic has helped more than 20 people complete the Sublocade regime. Today, those individuals are living successfully in recovery, unassisted by medication. Many more patients are actively in treatment and not using drugs.
“I see the system fail clients almost every day,” Gibbens said. “We have individuals who come in without a thing and don’t know how to navigate Medicaid or anything else. They just know they need help and want to be sober. So, I guess I am proud that I can now help anyone apply for Medicaid and begin treatment. [Applying for Medicaid] wasn’t a skill I ever thought I would need or develop. But if I can take down a barrier [to treatment], then I am excited I have the know-how.”
Taking the Next Step
Gibbens ultimately made it to recovery through MAT treatment at Urban Peaks Rehab. She started working at the clinic as a medical tech. Today, she manages all aspects of the office, whether marketing, providing emotional support for the patients, or billing insurance and Medicaid.
Taking the next step in her recovery, Gibbens recently started therapy. She is processing a lot, like the abuse she suffered as a child, experiencing homelessness off and on, and the ghosts of her years as an addict, including that day in the parking lot with her friend Natalie. That is one of the ghosts she cannot leave behind.
Natalie didn’t die that day in Duluth. Paramedics revived her with naloxone, a drug to treat overdoses. But Natalie didn’t seek treatment, and her luck ran out about a year later when she passed away from an overdose.
It would be impossible to describe Gibbens as selfish today. She doesn’t spend much time thinking about herself. Her focus is on giving second, third, and fourth chances to people who need help. She spends each day encouraging each patient as they go through treatment.
Gibbens also helps clients find housing, or sober living if they need it. The staff at Urban Peaks Rehab recognizes that many patients need more than medical treatment to become sober and move forward.
To seek help for addiction or learn more about Urban Peaks Rehab, visit urbanpeaksrehab.com.
Erika’s Story
Erica Gonzales finished her Sublocade treatment last March. Today, she works for Urban Peaks Rehab as a medical technician.
Gonzales said she began abusing drugs and alcohol because she wanted to feel numb. According to Gonzales, her family was unsupportive when she told them she was a lesbian at age 12. Gonzales’s dad died from suicide not long after.
“Dad was always around, he was just an alcoholic. He was a drug addict. And so, I’ve always seen that drug addiction side of life,” Gonzales said.
She blames herself for his death. Her parents had split up, and her father asked her if she believed there was a chance that her mom would take him back. Gonzales said no and watched him deflate. The next day, he took his life.
Gonzales understands that a 12-year-old isn’t responsible for taking care of their parents, but she can’t shake the thought that she hurt him.
“You can’t take that back. Words are powerful. So. I have to live with that,” she said.
Gonzales began drinking heavily around that time. She began using Percocet when she was in her early teens, stealing it from her mom’s purse and medicine cabinets. By age 14, Gonzales was taking Percocet daily.
“Percs were the comfort I’d been looking for,” Gonzales said. “I no longer felt guilty [about being a lesbian and my father’s [death] when I was high. I felt no shame, guilt, nothing. That’s just something I continued to chase until it became a living hell.”
Gonzales switched to oxycodone when it was too difficult to find Percocet. Then she smoked heroin when the pills became too expensive. At age 15, she injected heroin for the first time.
“I knew I shouldn’t have done that,” Gonzales said. “I could tell that black cloud was going to follow me, and that shadow followed me everywhere. After the [first] hit, I remember waking up wanting to do more. I just thought, ‘Is this what it’s like? Is this what heroin addicts feel? Am I one now?’”
After being expelled from high school for dealing drugs, and being hit with multiple arrests for shoplifting, Gonzales entered rehab. After three weeks, Gonzales had her dealer pick her up.
She tried MAT at another clinic but felt the doctors didn’t care about her. They rushed her out of the office with a prescription but no support.
“It was a bad experience because you’d sit there for an hour and see the doctor for like five minutes,” Gonzales said. You could tell they didn’t give a shit. They just saw you as an addict and nothing more.”
Gonzales eventually stumbled into Urban Peaks Rehab and began Suboxone treatment. But she didn’t stop using. Instead, Gonzales timed her heroin use around the Suboxone.
It was Sally Gibbens, along with former Urban Peaks Rehab staff member Brittany Kitchens, who helped Gonzales commit to her treatment and stop using. And when the office needed a new medical technician, Gonzales applied.
“I don’t think Doc [Johnston] was sure about hiring me,” Gonzales said. “I think he was the most skeptical because he knew me. I was just a shitshow when I started here. But once I was given the opportunity, it gave me something I didn’t have… something I needed.”
Gonzales said she knows the most important part of her job is being available to help others as they go through treatment. She doesn’t believe she would be sober without the personal connection she built with Urban Peaks Rehab staff.
“As much as Sally and Brittany were there for me, that’s what I’m trying to be to [current patients],” Gonzales said. “A lot of the people just feel abandoned. Like they don’t matter in this world. That’s how addicts feel. You can get to where you feel like, ‘What’s the point? It’s easier to die than get better.’ People are tired of trying. I just try to be here for addicts when they feel that way. I get on their level with them and I tell them I was an addict too. It gets better.”
While Gonzales is still building her life, she said she is content that she has a home and a job. She has security that she had never experienced before and worked hard to get this far.